GMC : Group Mediclaim (self + spouse +2 children)
GPA : Group Personal Accident (self)
Mediclaim providers
- Insurance companies
- Third Party Insurance Agents
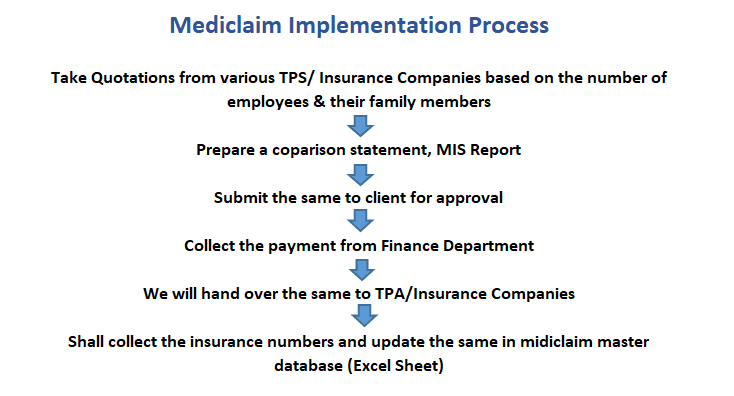
Mediclaim implementation process
We have implemented Mediclaim for some of our clients. Initially we will take the quotations from various TPS or insurance companies, based on the number of employees and family members. After that we will prepare a comparison statement MIS Report and will submit the same to the client for approval. After getting client approval we will collect payment from finance department from our client and we will handover the same to TPA.
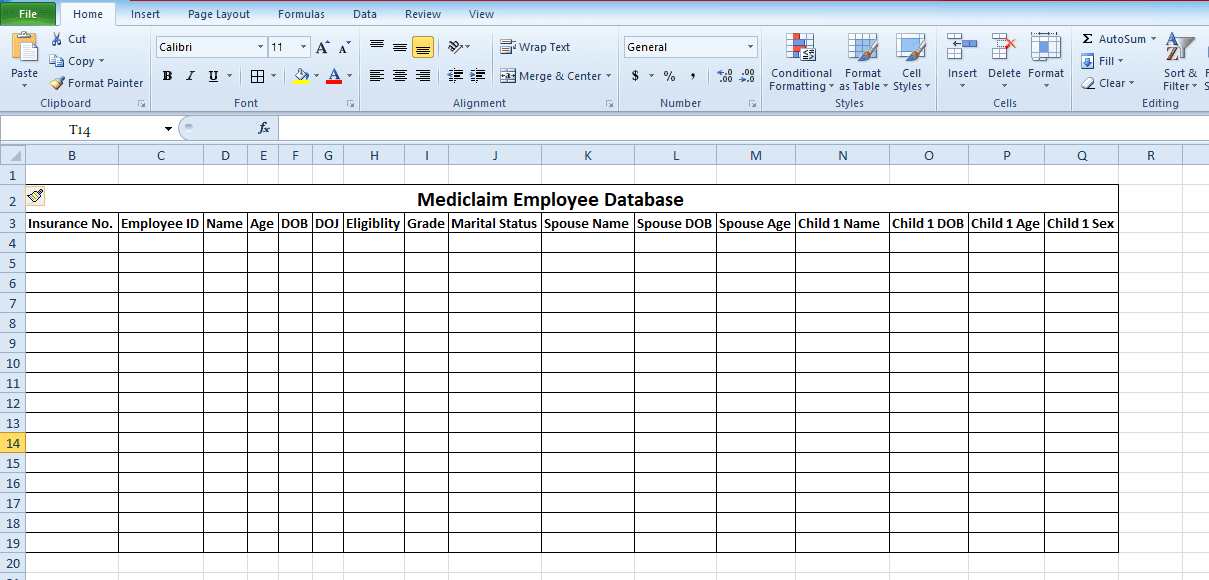
We will collect the insurance numbers and will update the same in Mediclaim master database excel sheet .
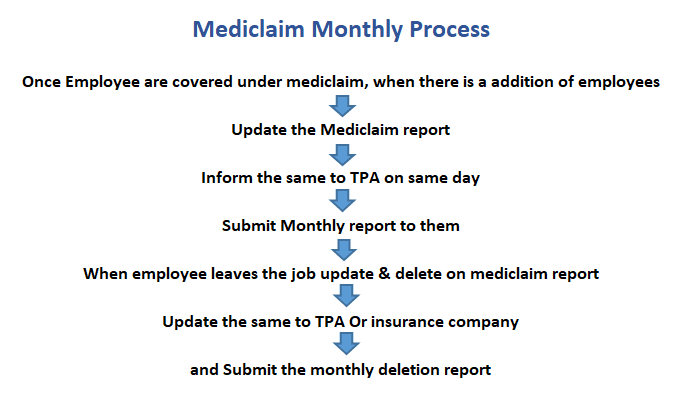
Mediclaim Monthly Process
Once the employee is covered under Mediclaim and whenever there is an addition of new employees, spouse or children, we will update Mediclaim addition report and we will inform the same to TPA insurance company on the same day and will also submit monthly reports to them.
When employees are leaving the job we will update the Mediclaim deletion report and update the same to TPA or insurance company mediately and submit monthly deletion report to them.
If the new joining employees are more in number, TPA will raise an invoice to us for extra payment, we will collect the amount from our client and release the same as soon as possible.
Mediclaim Full & Final Settlement
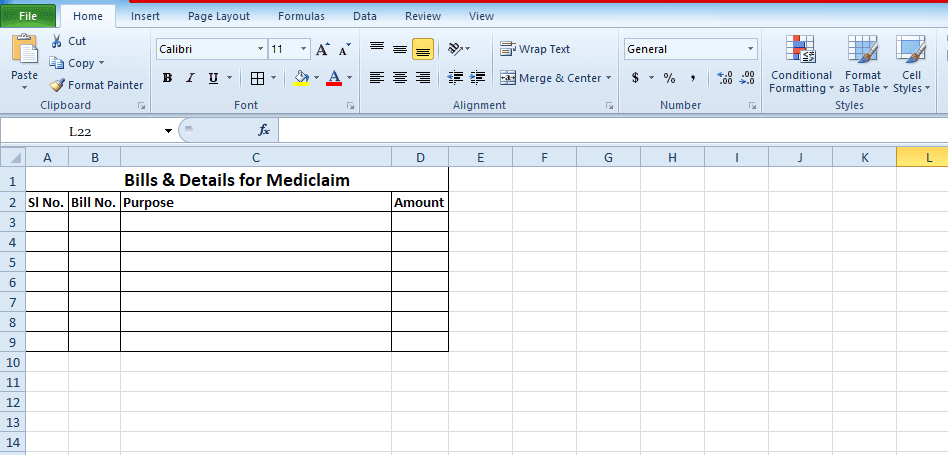
Documents required for Mediclaim settlement
- Claim application form
- Mediclaim insurance card copy
- Bills checklist for the amount to be claimed
- Discharge summary
- Discharge certificate
- X-Ray original
- All bills & documents original as per checklist
- Any other supporting documents from Hospitals
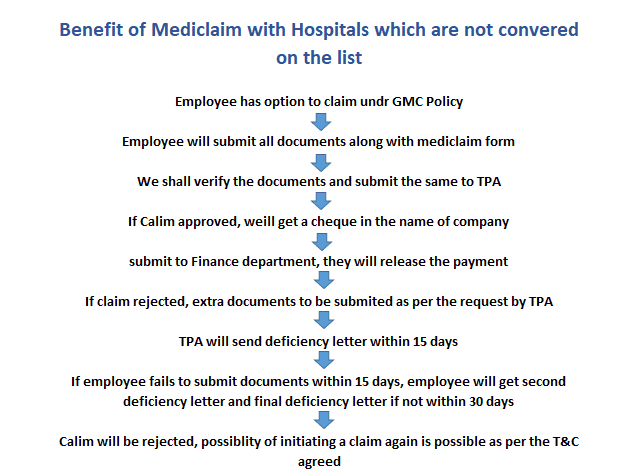
if the employee availed the medical benefits with hospitals which is not covered under medical policy, employee has the option to claim the amount under GMC policy.
Employee will submit all necessary documents along with Mediclaim form to us, we will verify the documents and will submit the same to TPA for approval.
Employee should furnish the documents and details as stated below
If the claim is approved by TPA or insurance company they will release the checklist amount in the name of the company and we will submit the same to finance department and then the amount will be released to the employee as a payment.
If the claim is rejected, extra documents to be submitted by employee, TPA will send a deficiency letter to employee for which they have to reply and submit the deficiency document within 15 days. if the employee doesn’t submit the documents within 15 days, they will send the second deficiency letter and final deficiency letter in next 30 days. If the employee is unable to submit the documents within 45 days, claim will be rejected and all the original bills and documents will be returned back to the employee.
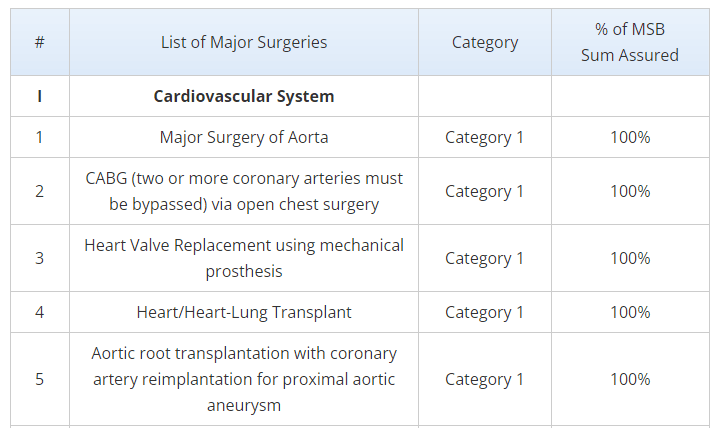
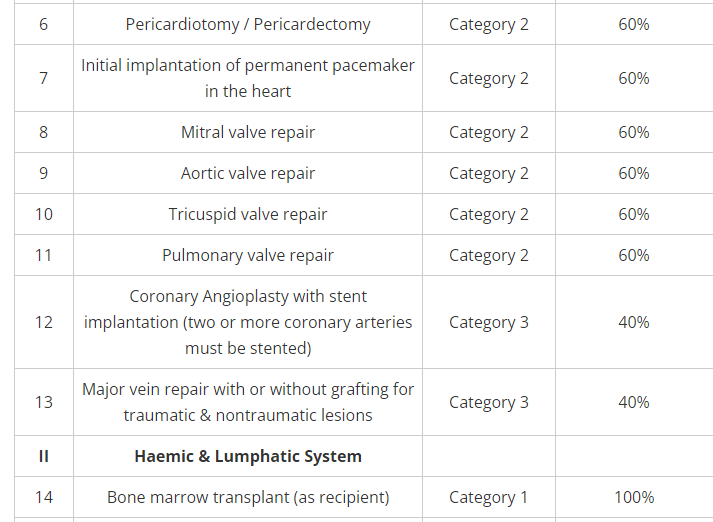
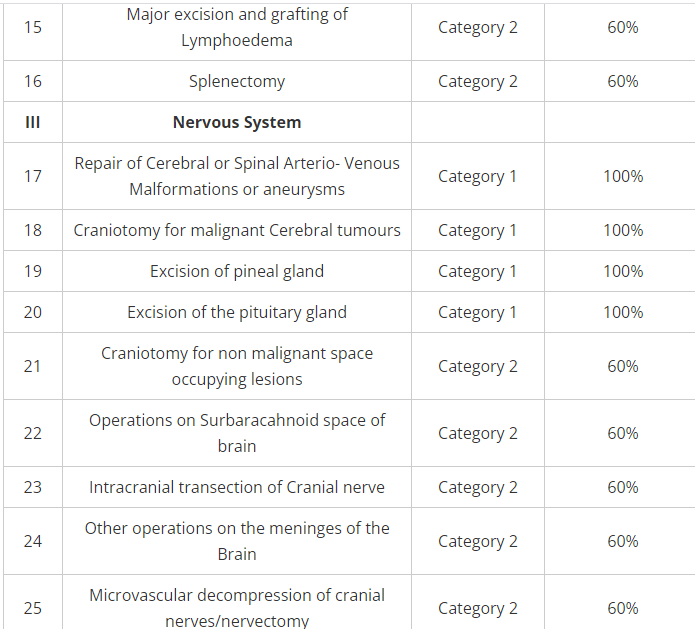
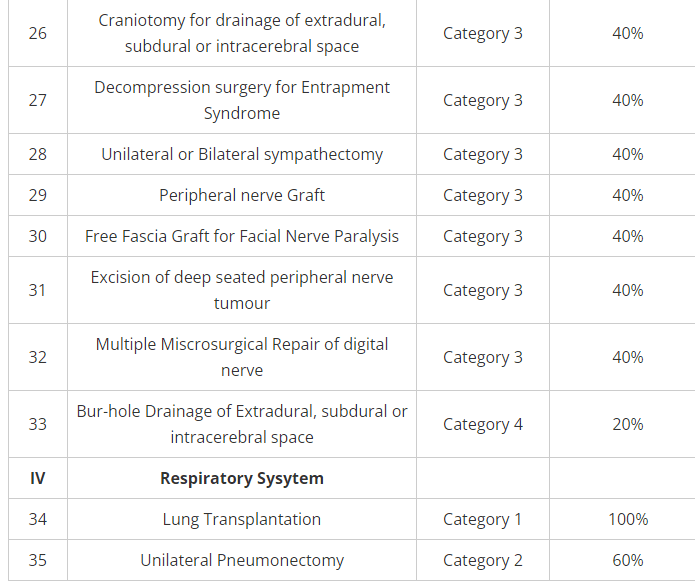
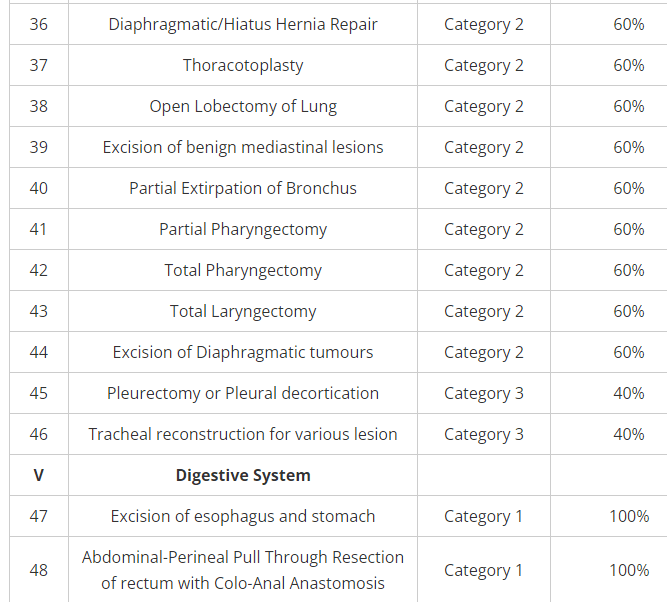
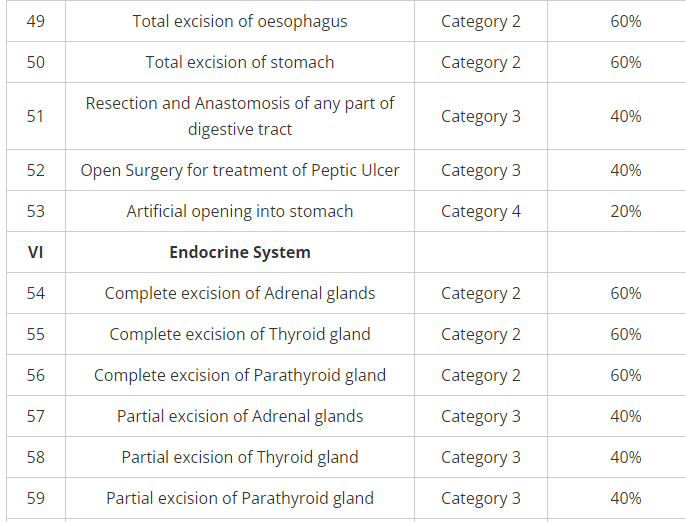
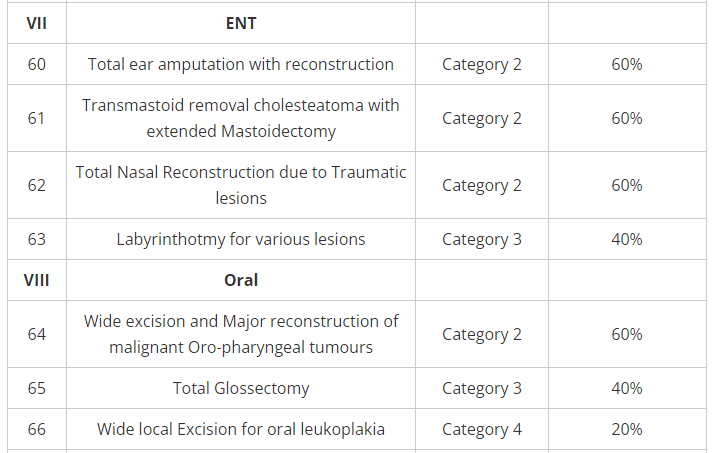
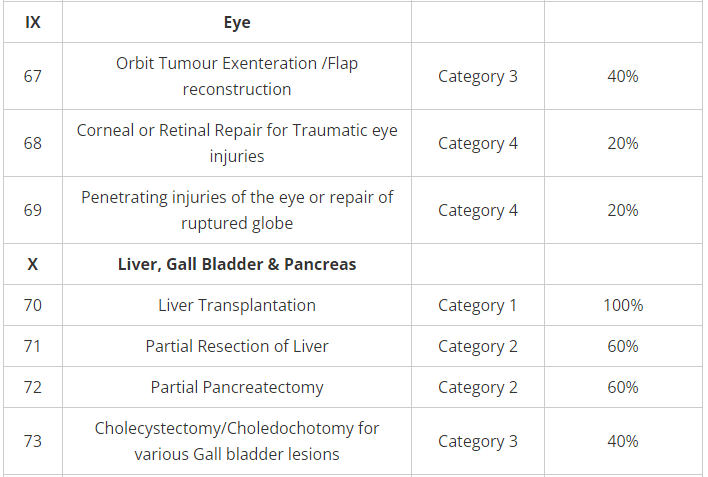
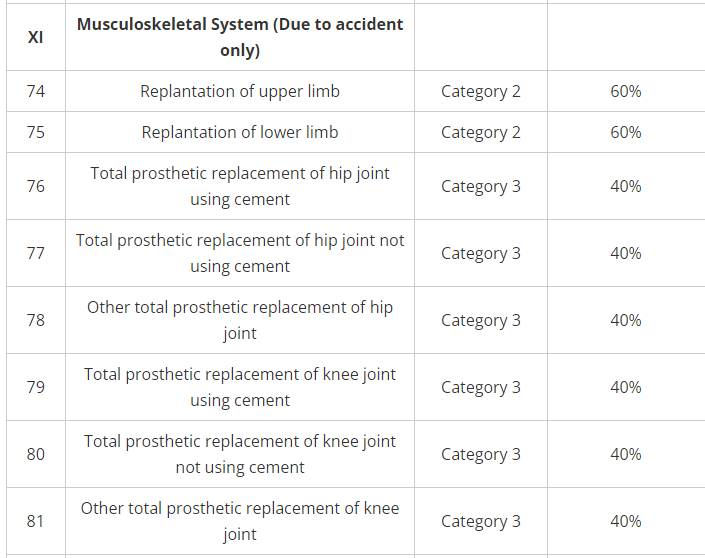
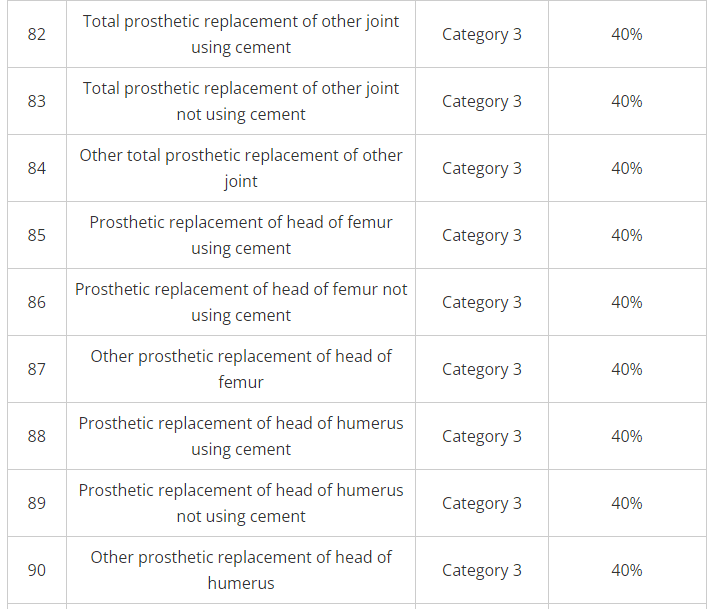
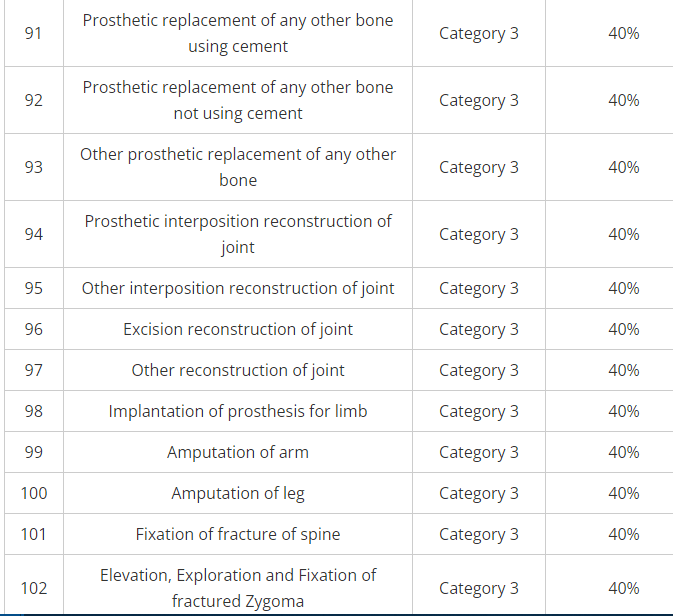
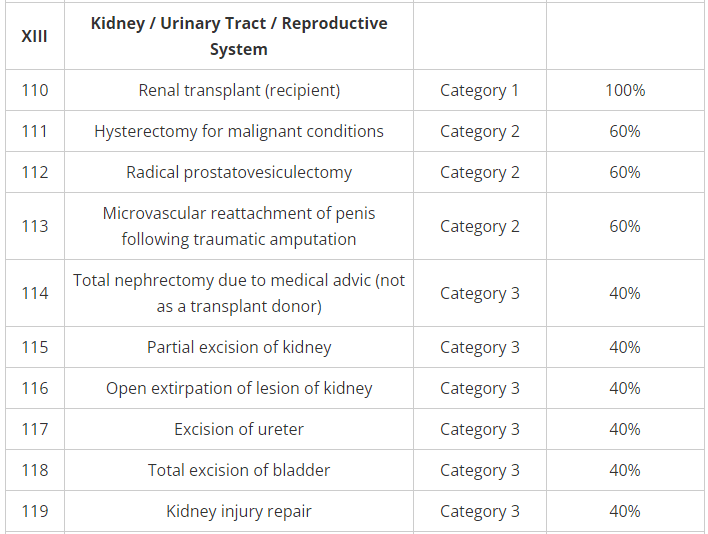
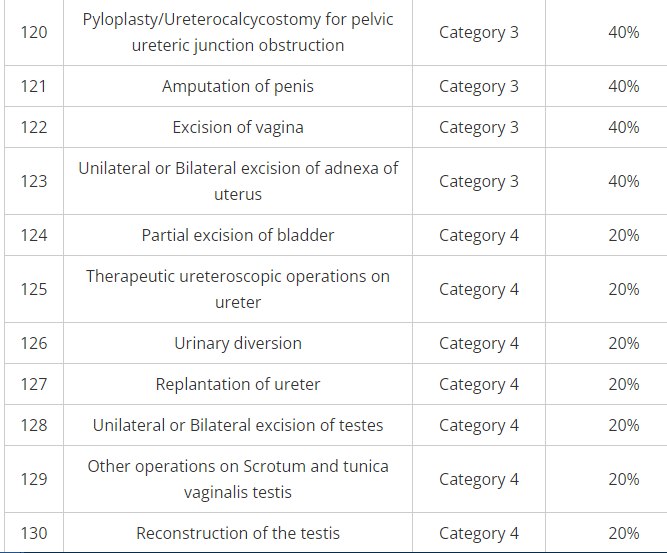
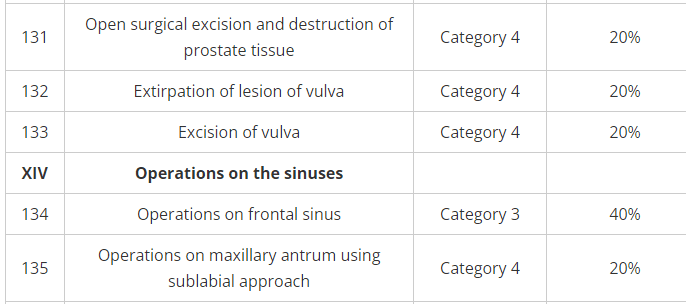
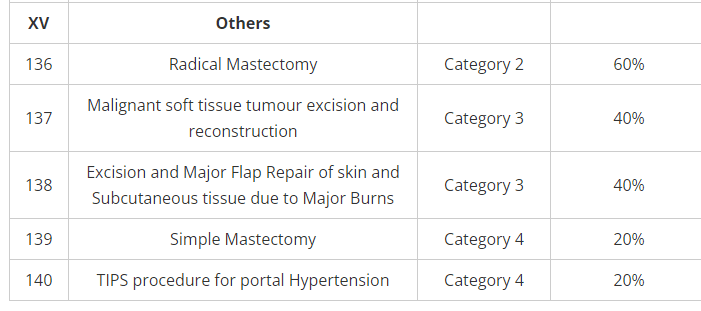
Sample of TPA list of diseases and percentage of coverage for each of those